How Lean Thinking and Switch Change Management Benefits Small Healthcare Practices

Many successful Advanced Primary Care models have been implemented in community clinics or staff models where extended health care professionals, including nurses, health coaches or social workers, are part of the existing interdisciplinary team. The Advanced Primary Care model could provide added value to independent physicians practices by improving patient-experience through team-based care while increasing work flow efficiency.
How to implement a standard care model within small practices, in which the physician is in charge and has limited staffing resources, is to be determined. This article will relate the application of ‘Lean Thinking’ and change management strategies based on the “Rider and the Elephant” theory from the book Switch by Chip Heath and Dan Heath, which describes the implementation of the Advanced Primary Care model at four diverse provider offices that still function as independent small practices. This article will show how the combination of ‘Lean Thinking’ application and evidence-based change management approach from the book Switch can benefit small practices
Introduction
Background
Primary care practices are under tremendous pressure by the health care industry to do more with less, while demonstrating high quality outcomes. The passage of the Affordable Care Act1 ushered in the Triple Aim as coined by Dr. Don Berwick, the former Center for Medicare and Medicaid (CMS) Director and Founder/CEO of the Institute for Healthcare Improvement (IHI.) Dr. Berwick stated that improving the U.S. health care system requires simultaneous pursuit of three aims:
- improving the experience of care
- improving the health of populations
- and reducing per capita costs of health care. (2)
The principles behind improving the patient’s experience of care is very consistent with what successful service industries have known for decades.
Creating a service experience that exceeds the customer’s expectation, is the key to quality and profitability. The United States will not achieve high-value health care unless improvement initiatives pursue a broader system of linked goals.
Creating a service experience that exceeds the customer’s expectation, is the key to quality and profitability. The United States will not achieve high-value health care unless improvement initiatives pursue a broader system of linked goals. The implication for the primary care offices is to build capacity to create a positive patient experience at each visit, while addressing the overall health of the populations or the panel of patients assigned to their practices. Last, but not the least, the primary care provider offices must be able to provide more value-added services with less financial resources. The good news is that the daunting dilemma faced by the US health care industry today have been solved by other industries such as Toyota’s experience, as described in the book Lean Thinking. (3) James Womack and Daniel Jones successfully translated the Toyota Production System, which combines operational excellence with value–based strategies to a Lean methodology, for adaptation to other industries.
This article will describe the experience of Best In Class (BIC) Physicians Group, deploying the Lean methodology in its adaption of the Advanced Primary Care model. This case study will emphasize the “change management” approach embedded in the BIC’s transformational journey to achieve the Triple Aim.
About the Best in Class (BIC) Physicians Group
The BIC Physicians Group consists of several traditional independent Board Certified physicians practicing in a culturally diverse Elsewhere county, USA. These physicians come together as part of an Independent Practice Association (IPA) in order to gain economies of scale by sharing administrative support services such as contracting, billing, practice management, and electronic health record systems support. Despite the fact that BIC is considered one single business entity, the physician offices continue to function separately with many variations in clinical and administrative processes.
In order for BIC to compete in the local market, it now needs to differentiate itself as the true “Best-In-Class” physicians group to gain back market share of patients with Medicare and Commercial health coverage.
Each BIC office has a loyal following of patients whom have developed trusted relationships over the years with the physicians and the office staff, however, other reputable medical groups have recently expanded their market into BIC’s territory in Elsewhere county. BIC began to experience a slow erosion of its membership base to the new groups as patients changed insurance coverage. In order for BIC to compete in the local market, it now needs to differentiate itself as the true “Best-In-Class” physicians group to gain back market share of patients with Medicare and Commercial health coverage. BIC physician management decided that in order to better compete, the offices must transform into Patient-Centered Medical Homes having standardized Advanced Primary Care practices, while retaining each physician’s unique style that attracted its current loyal patient base.
Primary Care Landscape Shifting to Patient-Centered Medical Home Model
The “Medical Home” is a concept coined in 1967 by the American Academy of Pediatrics and expanded over time as the “Patient-Centered Medical Home (4).” More recently, CMS approved the demonstration of the Advanced Primary Care (APC) model in the Federally Qualified Health Centers (FQHC.) The APC model relies on the use of physician or nurse practitioner lead collaborative teams of health professionals to provide patients with comprehensive and personalized primary care. According to CMS, medical care under APC requires a “shift from an acute care complaint-driven primary care paradigm,” which fragments health care delivery to one that is geared to maintain the patient’s overall health and anticipates when additional services or coordination needs to occur.” (5, 6)
Regardless of the “name du jour,” as the Affordable Care Act (ACA) unfolds, the key concepts of the “Medical Home” or “Advanced Primary Care” remain consistent describing a health care service delivery model in which the patient/consumer chooses a primary care setting (that may include specialty care services) as the basis for accessible, continuous, comprehensive, and integrated care. The interdisciplinary health care team provides evidence-based services from health management to disease prevention, matching an individual patient’s health care needs while coordinating with other services within the community. Instead of treating illness as the primary focus, the team proactively addresses the health care needs of its panel of patients, through proactive health risk screening and continuous improvement, driven by quality performance indicators. For the sake of consistency, this article will use the term “Advanced Primary Care” instead of the more familiar but slightly outdated “Medical Home.”
Many successful Advanced Primary Care models were implemented applying Lean techniques, adapting the Toyota Production System and the Six Sigma improvement approach in the community clinics or staff models.
Many successful Advanced Primary Care models were implemented applying Lean techniques, adapting the Toyota Production System and the Six Sigma improvement approach in the community clinics or staff models. The Group Health (7) experience has been a well-cited experience and success story of the Advanced Primary Care model.Group Health clinics’ health care professionals (including physicians, registered nurses, health coaches, and social workers) are part of the interdisciplinary team in the clinics.
Since BIC Physicians Group is the largest Independent Practice Association in Elsewhere County, the Advanced Primary Care model could provide added value to the independent practicing physicians’ offices. Implementing such a paradigm shift in the traditional small practices, in which the physician functioned as the “boss” with limited staffing resources (consisting of mostly Medical Assistants), still has yet to be determined.
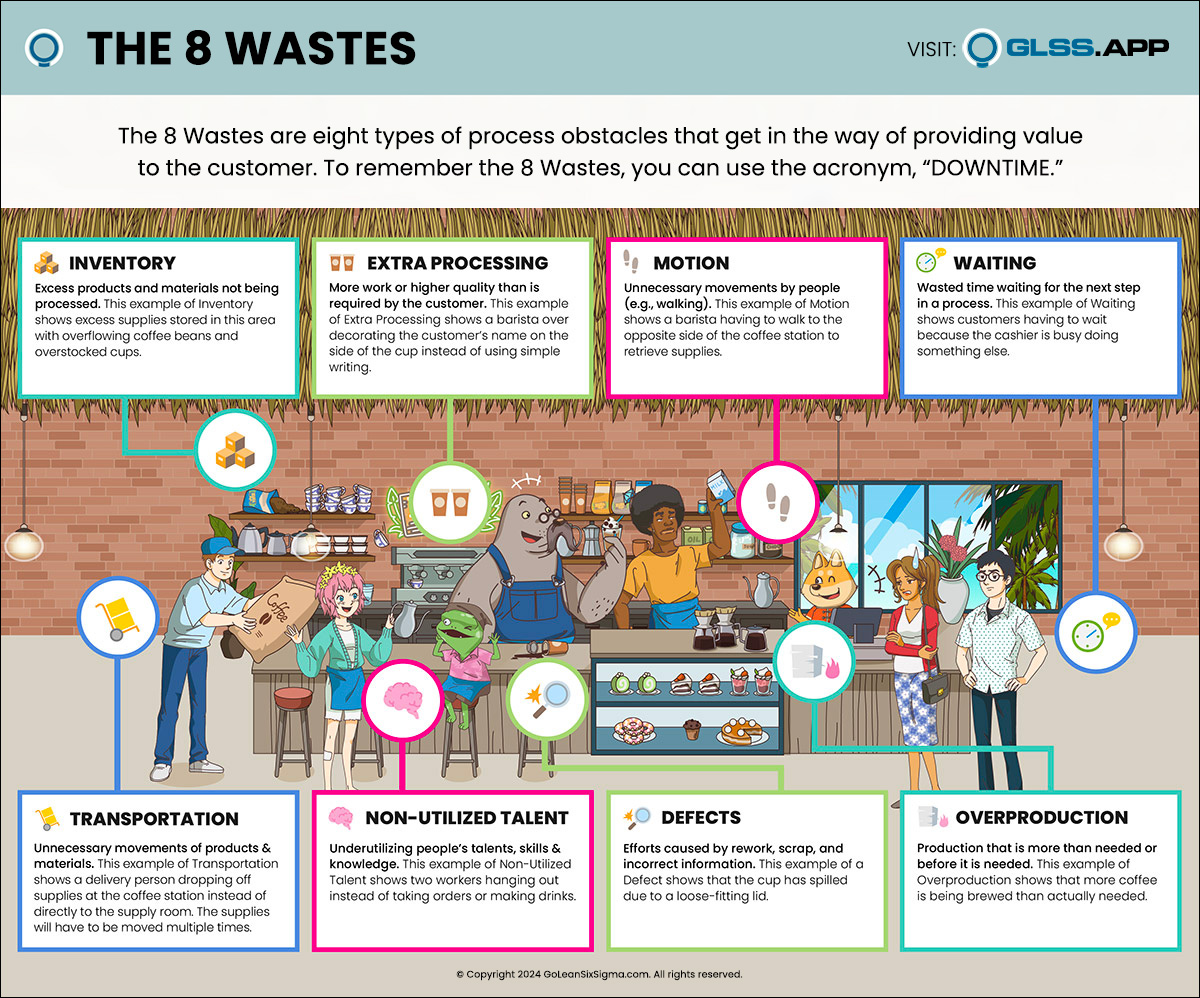
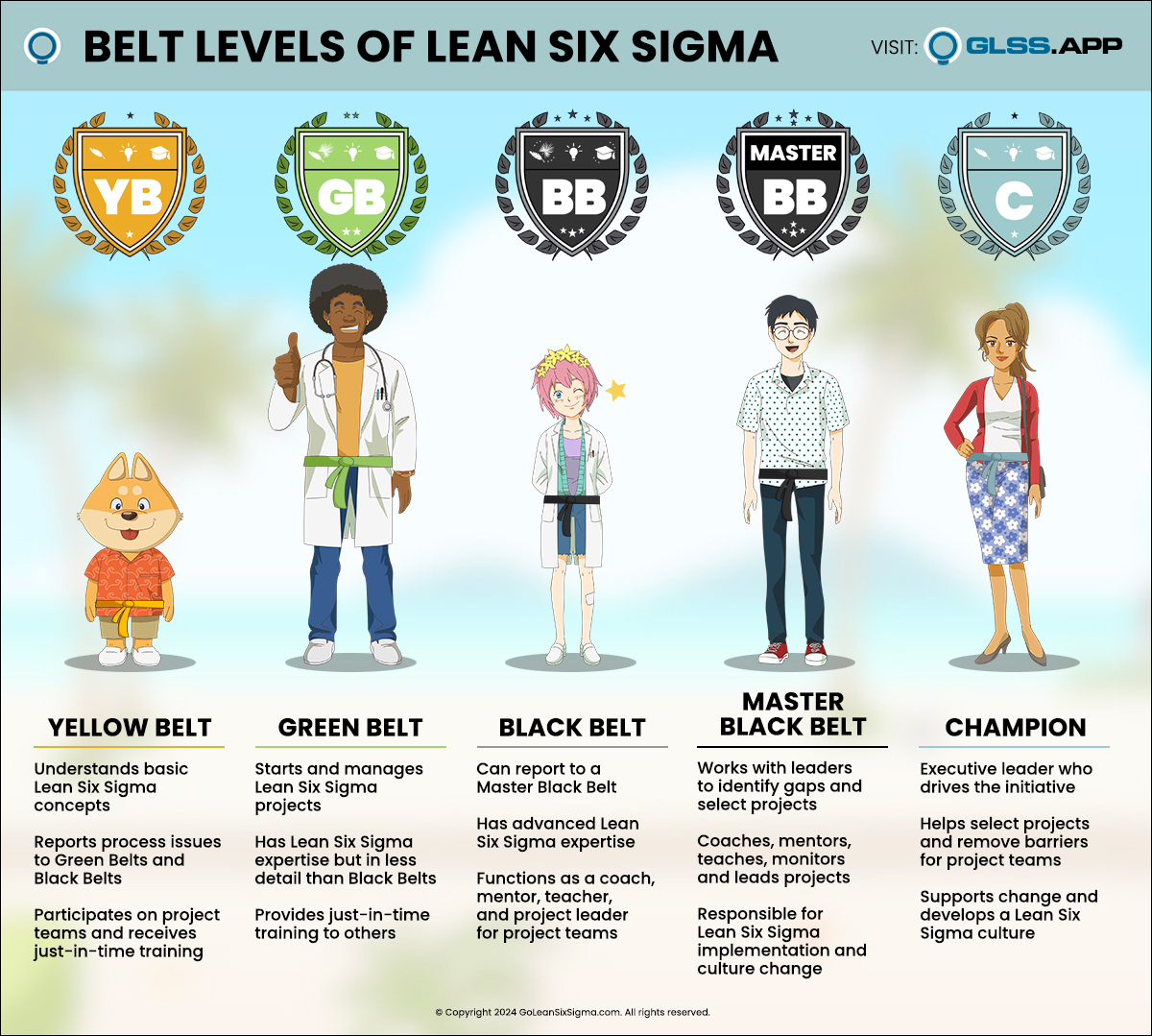
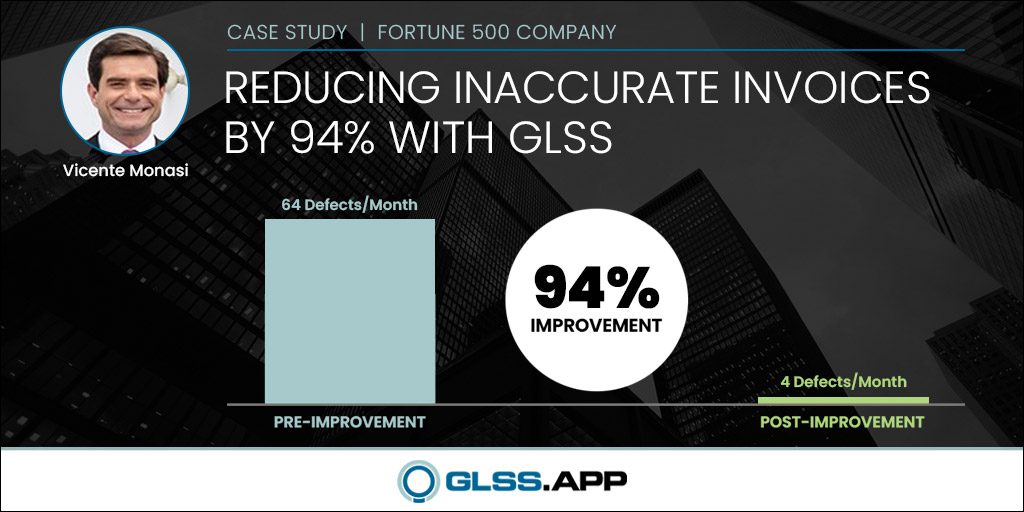
Since the literature has provided evidence of the efficacy of applying Lean techniques and Six Sigma methodologies, BIC physician managers chose to apply Lean methodology in the Advanced Primary Care model pilot in four very different provider offices. Additionally, they employed a Lean Six Sigma Master Black Belt consultant to train the providers and office staff to transform its operations to increase quality and efficiency by eliminating wasteful processes.
Current State
The Voice of the Customers
After the initial kick-off event that included key stakeholders, BIC physicians and physician assistants, the consultant conducted on-site staff training followed by a full-day Gemba Walk (8) at each office. The Gemba Walk process was designed to observe and document the current state from the patient’s perspective and experience. The consultant also interviewed the patients during their wait time to capture the Voice of the Customers (VOC). Table I summarizes the VOC from the four offices:
Table 1. BIC Voice of the Customers (below)

The Challenges
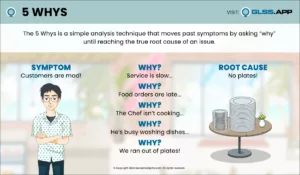
There are several challenges in applying the Lean approach to transform the BIC provider offices.
The first challenge was the time constraint of the offices. In the Toyota practice, the frontline workers are pulled off the production line to conduct Kaizen events over several days. But, implementing Kaizen–like events at provider offices can only be done during lunch time over a one to two hours maximum timeframe, to minimize interruption to the patient visits. The consultant had to be flexible and creative in condensing the Lean training into nuggets and deliver just-in-time actionable information. This condensed “crystalized” approach enabled the office staff to absorb the new concepts quickly and apply to tasks in real time, promoting active collaborative learning experience.
The consultant had to be flexible and creative in condensing the Lean training into nuggets and deliver just-in-time actionable information. This condensed “crystalized” approach enabled the office staff to absorb the new concepts quickly and apply to tasks in real time, promoting active collaborative learning experience.
The second challenge was how to gain efficiency leveraging technology and standard processes among the providers from diverse generations and age ranging from baby boomer to generation X. For example, a standard process of documenting in the electronic health records during the patient visit and creating a complete patient plan by the end of the visit can be a monumental challenge for the physicians who never learned to type and are not comfortable using the computer during the face-to-face patient visit.
The third challenge was how to gain consensus among the physicians to one “best practice” when each physician views his/her office as the very best amongst peers.
Opportunity for Change
The Switch
The key concept of the book Switch by the Chip Health and Dan Heath is “how to change things when change is hard.” (9) Switch successfully translated evidence-based change management theories into practical application, taking into consideration that our minds are ruled by two different systems – the rational mind, represented by the “rider,” and the emotional mind, represented by the “elephant”– that compete for control. (9)
The consultant applied these principles as part of the key change management strategies in the Lean transformation of the four BIC practices.
How We Direct the Rider – The Logical Mind
Find the Bright Spot
Many of us aspired to be a doctor in high school, but few of us make it into medicine. Typically, the best and brightest students get accepted into medical school. It takes determination, dedication, and hard work to complete the medical training and residency to become a physician. The BIC physicians are also Board Certified, running their own small practices as successful entrepreneurs.
There is a certain pride and passion about practicing medicine independently. Therefore the consultant’s first step was to harvest the bright spots and showcase what is working well in these offices that can be replicated. For example, one doctor consistently delighted the patients by remembering special information about the each patient, such as who referred them, special life events, and interests.
The physicians simply utilized the “sticky notes” feature of the electronic health record to document personalized information about the patient and pulled them up during each patient visit. All the medical assistants were trained to utilize the “sticky notes” to deliver personalized services. One office minimized the perception of waiting time by moving the patient into an exam room as soon as one is available and prepared the patient for the physician visit. The constant personal contacts and continuous flow of services minimize the patients’ perception of a long waiting time for their doctor. Another office sought to improve the experience of the patients’ parent by accommodating a group visit of several siblings at one time for well-child care, primary to school starting. Many of these bright spots can be incorporated into the Advanced Primary Care model.
Script the Critical Moves
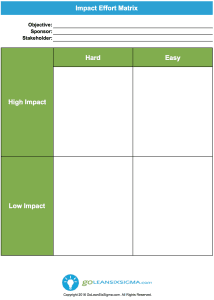
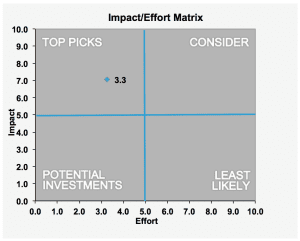
There are many change elements required to be certified as a Patient-Centered Medical Home by the National Committee of Quality Assurance (NCQA.) To tackle all the requirements at once can be daunting. The four pilot sites were given a listing of Advanced Primary Care change elements (termed a ‘menu’) to consider at the start of the process.
After conducting the Gemba Walk, harvesting the bright spots, and presenting the findings to each individual office, the consultant then convened a Think Tank of the physician champions, physician assistants, medical assistants, and office managers to review the current state and reach a consensus on standard processes and works. Then, the Think Tank participants presented the proposed standard activities categorized by before visit, during the visit, and after the visit to respective office teams for additional feedbacks.
The collective document is converted into a roadmap for the BIC office managers to follow- through in collaboration with each office team. For example, one of the scripted moves on the roadmap was how to conduct a five-minute daily huddle at the office. A standard checklist, including who should be present at the huddle, and what should be discussed was to be created and implemented at each office.
Point to the Destination
The destination of this initiative was clearly articulated from the start at the kick-off meeting by one of the most respected physician leader. He painted a vision that BIC is going to be the best-in-class premier medical group in the local market offering Advanced Primary Care model leveraging electronic health records in each offices with efficient standard processes and standard work. BIC aims to be the provider offices of choice with Five Star rating and be in the top quartile in quality performance among the IPAs in the national market.
How We Motivate the Elephant – The Emotional Mind
Finding the Feeling
People, who choose the health care career, typically are mission-driven and compassionate individuals who find purpose in their professional work. As health care becomes a commodity traded on Wall Street, and the payers start to drive how health care service is delivered instead of by the physicians, many health care professionals including the physicians become discourage or disenfranchised. To help the BIC providers to find the feeling, they were asked to imagine the ideal health care visit for their Grandmother.
The BIC providers realized that they are part of the larger health care reform effort with the responsibility to fix the unsustainable health care system for our future generations.
How should we transform BIG’s office, so they would choose BIC for their loved one. The feeling amplifies the health care professional’s calling and responsibility to shape the future of health care for people we care about. The BIC providers realized that they are part of the larger health care reform effort with the responsibility to fix the unsustainable health care system for our future generations. The Advanced Primary Care prototype as developed through BIC’s transformation can be replicated to help other small practices.
Shrink the Change
In order to gain the non-pilot sites buy-in, two of the physician champions agreed to “sell” the BIC Advanced Primary Care model to the other BIC providers who were not part of the pilot. Instead of presenting all the details of the visits standard processes, the physician champions will propose two to three standard processes from each phase of the visits, including care coordination activities between visits to be implemented in all BIC offices during the next twelve months. The other providers will be given the opportunity to provide input and help shape the scope of change within realistic constraints of time and resources to demonstrate return on investment.
Grow Your People
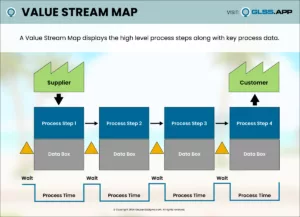
The BIC providers and staff are expected to be the best among the other IPAs. In addition to be identified as the best-in-class, the BIC pilot sites are often selected as innovation sites to test other new ideas. The pilot sites are empowered to identify improvement opportunities based on the Gemba Walk findings and Value Stream Map analysis. They were encouraged to apply rapid cycle improvement methodology and small test of change in their work areas. These small tests of change offered a safe opportunity to learn from failures and to recalibrate the next change effort using objective data. Failures were considered a necessary step of the learning process. Participating in the Think Tank shoulder-to-shoulder with the physicians gave the medical assistants the confidence to share their better ideas. The interdisciplinary Think Tank environment seeded a collaborative culture among the team and paved the ground for continuous quality improvement as BIC implement the Advanced Primary Care model as the best-in-class.
How We Shape the Path
Tweak the Environment
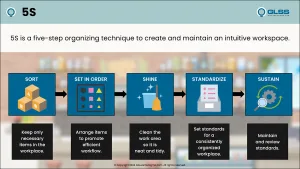
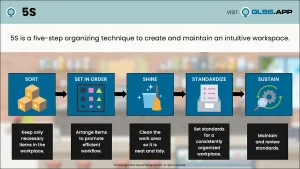
BIC offices are traditional doctor’s offices with a waiting room, front office, back office, and exam rooms. Most of the offices have limited space. During the Gemba Walk, wasted motion muda or waste was observed in several offices. For example, the printer is often placed far away, such as in the medical records room down the hall. The front office staff has to leave the front desk and walk down the hall to retrieve documents for the patient. A quick-win of tweaking of the environment was to move the printer at an arm’s reach distance of the front office staff. Patients often sit in the waiting room for a long duration waiting to see their doctor. One idea of tweaking the environment is to eliminate the waiting room completely, which was actually done successfully in other medical groups.
Build Habits
In order to build new habits and institute standards that reflect best-in-class primary care services, two tactics will be implemented to build new habits across the board. The first tactic is the humble check list. For example, the team will be trained to use a checklist to cover important topics during the daily huddle; a checklist of standard supplies and equipment to stock the exam room; and a checklist of in-office lab to be done for various types of patient visits. The second tactic is a standard script for all staff and patient communications to ensure a consistent patient-centered brand messaging. For example, a standard phone greeting script, an outreach script for preventive services, and a script for post hospital discharge calls.
Rally the Herd
The BIC Advanced Primary Care Lean initiative was rolled-out as the organization approaching its annual strategic planning cycle. The provider champions were invited to participate in the strategic planning process and define measures of success reflecting best- in-class performance of the BIC offices. These performance measures included results from elements of the Advanced Primary Care Lean initiative. The plan is to develop a transparent performance dashboard for each BIC office to show individual and team performance on a monthly basis. The dashboard will provide transparency among the peers and rally the herd to perform as BIC Physician Group name implies – the Best-In-Class!
Strategy to Keep the Switch Going
Under the shifting landscape of health care reform, transforming the small IPA provider offices in lightning speed to become best-in-class is no small feat. In order to keep the switch going at the BIC Physicians Group, additional wrap around support is clearly needed. The IPA organization of BIC plans to re-direct several corporate clinical professional staff to provide virtual and on-site support. For example, one case manager will utilize predictive modeling tools to help BIC providers identify and stratify patients by risk levels. The nurse case manager will also bring other discipline such as a social worker and clinical pharmacist to the patient care conference based on the patient’s care needs. The IPA medical director will help facilitate the weekly patient care conference for patients with complex high risk factors. The office managers will create a training program to re-train office staff on the standardized process and work across all BIC offices. The consultant will continue to serve as a sensei (teacher and coach) for BIC as it continues on this never-ending journey of seeking perfection.
Conclusion
Recognizing change is a dynamic process involving the rational mind and the emotional mind. It can be very helpful in implementing change in the health care sector. Change in the primary care providers’ offices involves motivating the highly educated physicians as well as the frontline medical assistants with minimal technical training. While Lean Thinking and sophisticated Six Sigma methodology are useful to implement improvement, effective change management can be expedited with the help of an objective facilitator or consultant who understand the intricacies of creating a change strategy that resonate with both the rider and the elephant; when the riders and the elephants move in unison, sustainable change will happen.
References:
- Patient Protection and Affordable Care Act, Health Related Portion of the Health Care and Education Reconciliation Act of 2010, Public Law 111-148 (2010). Retrieved from http://housedocs.house.gov/energycommerce/ppacacon.pdf
- Berwick, D.M., Nolan, T.W., & Washington, J. (2008) The Triple Aim: Care. Health, And Cost. Health Affair, 27(3), 759-769
doi: 10.1377/hlthaff.27.3.759 Health Aff May 2008 vol. 27 no. 3 759-769 - Womack, J.P., & Jones, D.T. (2003) Lean Thinking. New York, United States: Free Press.
- American Academy of Pediatrics. Retrieved fromhttp://www.medicalhomeinfo.org/publications/medical%20home.html
- Federally Qualified Health Center Advanced Primary Care Practice Demonstration Demonstration Design. Retrieved from http://www.cms.gov/Medicare/Demonstration- Projects/DemoProjectsEvalRpts/downloads/FQHC_DemoDescription.pdf
- Kurzweil, V. (2011, November 220. Re: CMS Demonstration to Test Efficacy of Advanced Primary Care Model, [RegBlog message]. Retrieved from https://www.law.upenn.edu/blogs/regblog/2011/11/cms-demonstration-to-test-efficacy-of- advanced-primary-care-model.html
- Reid, R.J., Fishman, A., Yu, O., Ross, T. R., Tufano, J. T., Soman, M. P., Larson, E. B. Patient centered medical demonstration: a prospective, quasi-experimental, before and after evaluation. The American Journal of Managed Care, 2009; 15(9): 71-87
- Gemba Walk Definition. Retrieved from http://en.wikipedia.org/wiki/Gemba
- Heath, C., & Heath, D. (2010). Switch. How to Change Things When Change is Hard. New York,United States: Broadway Books.